Rheumatoid arthritis (RA) is a challenging condition that many professionals encounter in their work. It triggers joint inflammation, damages cartilage, and disrupts patients’ daily lives. By improving synovial fluid’s lubrication and calming inflammation, hyaluronic acid (HA) offers a targeted approach to treatment. Let’s explore how HA works and what recent studies reveal about its potential.
Understanding Hyaluronic Acid
Keeping joints functional requires the right balance of lubrication and cushioning. That’s where hyaluronic acid comes in, serving as a natural shock absorber while supporting cartilage and hydration, for both osteoarthritis and rheumatoid arthritis. Understanding its essential role is the first step toward using it effectively in treatments.
Composition and Function
Synovial fluid relies on hyaluronic acid to remain thick and elastic, which is crucial for smooth joint movement and impact cushioning. Its impressive water retention also ensures joints stay hydrated and functional. HA has the ability to improve the viscoelastic properties of synovial fluid, directly influencing its biomechanical performance in weight-bearing joints.
Synthesis and Regulation
Hyaluronic acid is created by enzymes called hyaluronan synthases (HAS1, HAS2, and HAS3). These enzymes respond to inflammatory cytokines like IL-1 and TNF-α, often elevated in RA. When inflammation throws off HA balance, synovial fluid quality deteriorates, exposing joints to increased damage. Additionally, oxidative stress in RA patients further depletes HA, intensifying joint vulnerability.
Benefits of Using Hyaluronic Acid for Rheumatoid Arthritis
These properties collectively contribute to better mobility and an improved quality of life for patients.
Reduces Inflammation
Blocks harmful enzymes such as matrix metalloproteinases (MMPs) responsible for cartilage breakdown. Lowers inflammatory cytokines, including IL-6 and TNF-α, reducing joint swelling and tenderness. Calms synovial macrophages, decreasing chronic inflammation.
Protects Cartilage
Creates a protective barrier over cartilage, shielding it from mechanical wear and enzymatic damage. Promotes cartilage repair by improving the extracellular matrix environment. Prevents further degradation caused by inflammation and oxidative stress.
Enhances Joint Lubrication
Improves the viscoelasticity of synovial fluid, ensuring smoother joint movement. Reduces friction between articular cartilage surfaces during movement, alleviating pain and stiffness.
Delivers Targeted Relief
Injections focus treatment directly on affected joints, minimizing systemic side effects. Provides localized benefits for areas with acute damage or inflammation.
Suppresses Immune Overactivity
Modulates immune cell activity to reduce autoimmune attacks on joint tissues. Balances immune response, potentially slowing disease progression.
Reduces Oxidative Stress
Neutralizes free radicals in joint spaces, protecting tissues from further damage. Minimizes the impact of oxidative stress, a known factor in RA progression.
Improves Long-Term Joint Function
Delays structural damage, preserving joint integrity over time. Increases the overall range of motion, enabling better mobility.
Minimal Side Effects
Generally well-tolerated with few adverse reactions, such as mild injection site discomfort. Low immunogenicity compared to other treatments like biologics.
Enhances Multimodal Therapies
Complements other treatments such as corticosteroids, DMARDs, and biologics. Works synergistically in combination therapies to maximize symptom control and improve outcomes.
Broad Applicability
Effective not only for RA but also for overlapping conditions like osteoarthritis and joint trauma. Provides benefits for a wide range of patients, including those with moderate to severe joint damage.
Emerging Innovations
Advanced formulations such as HA nanogels and drug conjugates offer improved durability and effectiveness. Expanding into oral and topical applications for increased convenience and accessibility.
Patient-Centric Approach
Personalized HA-based treatments can be tailored to individual needs based on biomarkers and disease severity. Suitable for patients seeking alternatives to systemic drugs or those with contraindications to traditional therapies.
Rheumatoid Arthritis: Pathophysiology and Current Treatments
Rheumatoid arthritis is a complex autoimmune condition that demands an in-depth understanding of its biological mechanisms and current therapeutic strategies. This section explores the triggers and progression of RA, alongside evaluating standard and emerging treatments, setting the stage for integrating hyaluronic acid (HA) into patient care.
Disease Mechanisms
Rheumatoid arthritis arises from a cascade of immune dysregulation that primarily targets synovial joints. This condition is driven by an intricate interplay of genetic, environmental, and immunological factors. While T-cells and B-cells initiate and sustain inflammation, macrophages and dendritic cells are also important in exacerbating tissue damage. Beyond immune cell activity, fibroblast-like synoviocytes (FLS) amplify cartilage destruction by producing excessive matrix-degrading enzymes like MMPs and perpetuating inflammation.
Additionally, emerging research has linked gut microbiota imbalances to RA’s progression, suggesting that dysbiosis may fuel systemic inflammation. External triggers like smoking and infections can modify epigenetic markers, further increasing susceptibility. The presence of specific genetic markers, such as HLA-DR4 alleles, remains a cornerstone in understanding individual risk, yet environmental factors like obesity and diet are now being studied for their modulatory effects on disease severity. Altogether, RA’s mechanisms are multifaceted, combining immune-mediated destruction with structural and systemic vulnerabilities.
Standard Therapies
Current RA treatments include disease-modifying antirheumatic drugs (DMARDs), biologics targeting specific cytokines, and corticosteroids to reduce inflammation. While effective in slowing disease progression, these treatments often come with side effects, including immunosuppression, increased infection risk, and gastrointestinal complications, highlighting the need for adjunctive therapies like HA. In recent years, combination therapies have garnered significant attention, as they provide a tailored approach to managing rheumatoid arthritis (RA). Breaking these combinations down offers a clear picture of their potential benefits and patient-specific applications.
Biologics and Targeted DMARDs
Pairing biologics with targeted DMARDs addresses multiple inflammatory pathways simultaneously. For example, combining an anti-TNF agent with methotrexate can amplify the suppression of pro-inflammatory cytokines while minimizing joint damage.
Ideal for individuals with severe disease progression who have not responded to single therapies. Monitoring for overlapping side effects, such as infection risk, is crucial. Combining these therapies requires detailed patient history and close monitoring, as they increase the potential for immunosuppression.
Low-Dose Corticosteroids with HA Injections
Combining low-dose corticosteroids with HA injections provides immediate symptom relief while enhancing joint lubrication and long-term cartilage protection.
Particularly beneficial for patients experiencing acute flares with persistent synovial inflammation. Offers both quick and sustained relief. These combinations may allow patients to taper off corticosteroids more quickly, reducing the risk of long-term complications such as osteoporosis.
Lifestyle Interventions and Medical Therapies
Incorporating exercise programs, physical therapy, and anti-inflammatory diets alongside medical treatments creates a holistic approach. Exercise improves joint mobility, while diets rich in omega-3 fatty acids may reduce systemic inflammation. Combining lifestyle adjustments with HA and other medical therapies ensures better overall outcomes and patient satisfaction.
Best suited for patients with mild to moderate RA or those aiming to prevent disease progression through proactive management. This approach empowers patients by addressing modifiable risk factors.
The Holistic Approach
By integrating multiple modalities, including advanced pharmacological options and lifestyle changes, RA management becomes more comprehensive and adaptable to individual patient needs. This approach emphasizes not just symptom relief but also long-term disease control and improved quality of life.
Hyaluronic Acid as a Therapeutic Agent in RA
This section delves into how hyaluronic acid can be used to manage RA effectively. From its anti-inflammatory properties to its cartilage-protecting abilities, HA is proving to be a versatile option for treating joint damage and improving patient outcomes.
Mechanisms of Action
By blocking harmful enzymes and inflammatory molecules, different hyaluronic acid brands reduce joint inflammation and protect cartilage. It also regulates immune activity to minimize the autoimmune reactions driving RA. Additionally, HA has been found to suppress the activation of synovial macrophages and reduce oxidative stress, contributing to its overall therapeutic effect.
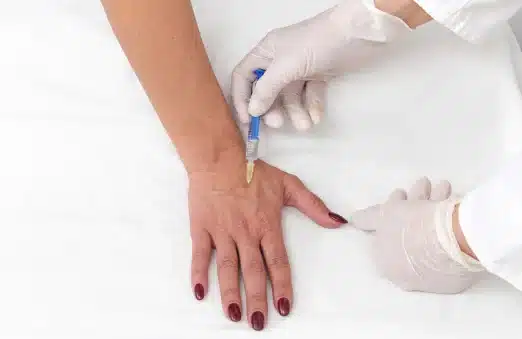
Delivery Methods
Hyaluronic acid is most often administered via injections directly into affected joints. This targets treatment where it’s needed most, reducing systemic effects. Emerging options like nanogels and HA-drug conjugates aim to make therapies longer-lasting and even more effective. Novel oral and topical formulations are also under development to enhance accessibility and patient compliance.
Additional Benefits Beyond RA
HA’s use extends to treating osteoarthritis and post-traumatic joint issues, which often overlap with RA. Its broad application in maintaining joint health further underscores its importance in musculoskeletal care.
Clinical Evidence and Research Findings
Understanding the clinical impact of hyaluronic acid is essential for professionals considering its use in RA management. This section examines research data on HA’s effectiveness, safety, and how it compares or complements other therapies in improving patient outcomes.
Efficacy Studies
HA injections reduced pain and improved joint function significantly over 12 weeks compared to placebo. Combining HA with low-dose corticosteroids provided even better pain relief and inflammation control. More recent meta-analyses have supported HA’s role in reducing the frequency of flares and improving long-term joint function.
Safety Profile
Orthovisc and Synvisc are among the best, as you can see in our comparison, but there are other good brands as well. Hyaluronic acid is generally well-tolerated, with minimal side effects. The most common adverse reactions include mild swelling or discomfort at the injection site. Long-term studies have shown no significant increase in systemic side effects, making HA a promising adjunctive therapy for RA management. The low risk of immunogenicity further adds to its appeal as a safe treatment option.
Innovative Approaches and Future Directions
Innovation in hyaluronic acid therapies is reshaping the landscape of RA treatment. Advanced techniques and technologies are broadening the scope of HA applications, offering more precise and effective solutions for joint health management. This section dives into cutting-edge advancements, from nanotechnology to personalized medicine, and their transformative potential in RA care.
HA Conjugates and Nanotechnology
Nanotechnology has opened new possibilities for delivering HA in more targeted and efficient ways. Researchers are exploring HA-methotrexate hybrids to deliver anti-inflammatory drugs directly to inflamed joint tissues, enhancing therapeutic precision. HA-coated nanoparticles are being developed to provide controlled and prolonged release of HA, ensuring consistent effects over time. These advancements not only improve bioavailability but also reduce the need for frequent injections, enhancing patient compliance and outcomes. Future innovations may include smart nanoparticles that respond to specific inflammatory markers, activating treatment only when necessary.
Personalized Medicine and Biomarker Integration
Personalized medicine is becoming a cornerstone of modern RA treatment. By integrating genomic, proteomic, and biomarker profiling, clinicians can tailor HA-based therapies to individual patients. For example, specific biomarkers linked to severe inflammation or cartilage degradation can help identify candidates who will benefit most from HA in combination with biologics or DMARDs. Machine learning tools and predictive analytics are also playing a role, enabling data-driven decisions about optimal treatment protocols and HA dosing.
Emerging Oral and Topical Formulations
While intra-articular injections remain the gold standard for HA delivery, emerging formulations aim to make HA treatments more accessible. Oral HA supplements are being investigated for their systemic anti-inflammatory effects, which could benefit patients with widespread joint involvement. Similarly, topical HA gels are being studied for their potential to provide localized relief for superficial joints, such as the hands and knees, making them ideal for patients with mild to moderate symptoms or as adjunctive therapy.
HA-Driven Multimodal Approaches
Combining HA with other therapeutic strategies is proving to be a game-changer in RA care. Multimodal approaches integrate HA with DMARDs, biologics, or physical therapy to tackle both inflammation and structural joint damage. For instance, pairing HA injections with targeted exercise regimens has demonstrated enhanced recovery of joint mobility and strength. Additionally, HA’s ability to improve synovial fluid quality complements physical therapies, reducing pain and facilitating movement during rehabilitation programs.
Sustainability and Future Innovations
The development of biosynthetic HA derived from sustainable sources is gaining traction, reducing dependency on animal-based HA. This approach aligns with the growing demand for environmentally friendly and ethically sourced medical products. Furthermore, researchers are exploring HA’s potential in regenerative medicine, including its use in 3D-printed scaffolds for cartilage repair, opening doors to entirely new treatment paradigms for RA and other joint-related conditions.
Conclusion
Hyaluronic acid offers a practical solution for improving joint health and reducing RA-related inflammation. As research advances, HA-based treatments and orthopedic injections in general will become a cornerstone of personalized care. For professionals, understanding the mechanisms, clinical evidence, and innovative approaches surrounding HA ensures informed decision-making and better outcomes for patients
References
Migliorini F, Maffulli N, Schäfer L, Kubach J, Betsch M, Pasurka M. Less Pain with Intra-Articular Hyaluronic Acid Injections for Knee Osteoarthritis Compared to Placebo: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Pharmaceuticals (Basel). 2024 Nov 20;17(11):1557. doi: 10.3390/ph17111557. PMID: 39598466; PMCID: PMC11597132.
Migliorini F, Giorgino R, Mazzoleni MG, Schäfer L, Bertini FA, Maffulli N. Intra-articular injections of ozone versus hyaluronic acid for knee osteoarthritis: a level I meta-analysis. Eur J Orthop Surg Traumatol. 2024 Nov 23;35(1):20. doi: 10.1007/s00590-024-04135-x. PMID: 39579218.
Sprott H, Fleck C. Hyaluronic Acid in Rheumatology. Pharmaceutics. 2023 Aug 30;15(9):2247. doi: 10.3390/pharmaceutics15092247. PMID: 37765216; PMCID: PMC10537104.
Saito S, Kotake S. Is there evidence in support of the use of intra-articular hyaluronate in treating rheumatoid arthritis of the knee? A meta-analysis of the published literature. Mod Rheumatol. 2009;19(5):493-501. doi: 10.1007/s10165-009-0189-6. Epub 2009 Jun 23. PMID: 19548064.
Chavda S, Rabbani SA, Wadhwa T. Role and Effectiveness of Intra-articular Injection of Hyaluronic Acid in the Treatment of Knee Osteoarthritis: A Systematic Review. Cureus. 2022 Apr 26;14(4):e24503. doi: 10.7759/cureus.24503. PMID: 35651409; PMCID: PMC9135165.


0 Comments